
I was told my new baby may have a hypospadias. Is it serious?
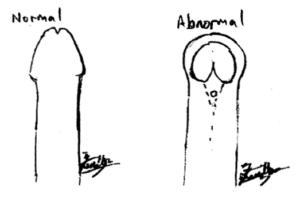
Hypospadias is an anomaly of the penis which includes, excess curvature (chordee), a hooded appearance of the foreskin, deficient foreskin on the bottom side of the penis, an abnormal urinary tract opening (urethra meatus) and a rotational abnormality of the penis. It affects up to 1 in 100 boys (1). It causes spraying of urine, wets the pants when the child is standing to pee, and curved erection (chordee) which can be painful. Thankfully, hypospadias is not life threatening, and not commonly associated with other anomalies.
What are the other anomalies associated with hypospadias?
A proximal hypospadias can be associated with undescended or absent testis(es), disorder of sex development, abnormalities of the scrotum for example, bifid scrotum or penoscrotal transposition. These should be diagnosed and managed by a paediatric surgeon or pediatric urologist.
Can medicine cure hypospadias?
No, hypospadias is corrected only with surgery to ensure normal urine and sexual function. Testosterone pre operatively can increase penile length and width, but there are side effects (2). These include the risk of masculinization, agitation, increased bleeding during the surgery and worse scarring post op.
When is the best time to correct hypospadias?
The best time is before the child becomes aware of himself, to minimize the psychosocial effect of the condition. Although hypospadias repair was classically proposed to be performed from 6 months to 18 months old, repairs done later than 18 months old have been shown to have similar form and function post surgery (3).
What happens during hypospadias repair?
Hypospadias repair is performed under general anaesthesia. The aims are to: 1) correct the excess curvature (chordee) via orthoplasty, 2) bring the urinary opening to the tip of the penis by creating a new urinary tract (urethra reconstruction / urethroplasty) and, 3) repair any rotation anomaly. During the urethroplasty, a urinary catheter is inserted as part of the surgery. A dressing is placed over the penis and needs to be kept on.
When it is a proximal hypospadias (urethra meatus at the penoscrotal or scrotal position after orthoplasty), and the skin is sufficient to perform the urethroplasty, I perform a single stage repair. A temporary urinary catheter and dressings are used for the reconstruction.
However when the available skin for urethroplasty is not enough, the skin is stitched to the ventral surface of the penis and left for 6 months. Six months later, the 2nd stage hypospadias repair is performed by creating a new urinary tract out of the ventral foreskin.
The risk of complications of hypospadias repair e.g. dehiscence, stricture and fistula are higher with a proximal hypospadias.
How is the follow up care post hypospadias repair?
Hypospadias repair is usually performed as a day surgery procedure. Alternatively, the patient can have an overnight stay for observation. When the parents / caregivers are confident with the catheter and dressings care, the child can be managed at home. It is important to prevent him from pulling off the catheter or dressings. Minimal bleeding is expected. Please ensure he drinks enough and passes soft stools, because these help to relieve any discomfort. Clear urine in the catheter is a good marker that he is well hydrated.
The dressings will be removed on post op day 2 to 3, and the catheter at post op week 2 to 3. I advise my patients to excuse physical exercise and swimming for at least 3 weeks.
In a 2 staged hypospadias repair, the 2nd stage is performed 6 months later. This allows the skin to heal well and mature for the reconstruction of the new urethra opening. Post op care is similar to a single stage repair.
References:
1. van der Horst HJR, de Wall LL. Hypospadias, all there is to know. Eur J Pediatr. 2017 Apr;176(4):435–41.
2. Chua ME, Gnech M, Ming JM, et al. Preoperative hormonal stimulation effect on hypospadias repair complications: Meta-analysis of observational versus randomized controlled studies. J Pediatr Urol. 2017 Oct;13(5):470–80.
3. Bush NC, Holzer M, Zhang S, et al. Age does not impact risk for urethroplasty complications after tubularized incised plate repair of hypospadias in prepubertal boys. J Pediatr Urol. 2013 Jun;9(3):252–6.
Share if you like this post
If you have other enquiries on children’s surgical conditions, feel free to contact us
© Copyright- 2020 Childsurgery.sg
All Rights Reserved