Table of Contents
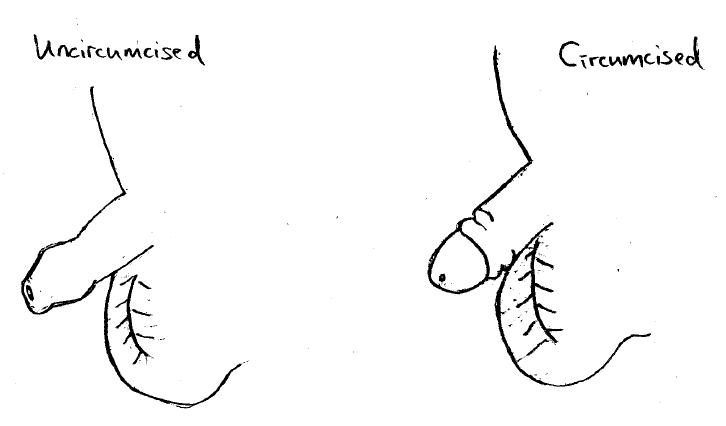
What is circumcision?
Circumcision is the removal of the excess foreskin of the penis. It is the treatment of choice for a foreskin that is stuck behind the head of the penis (paraphimosis). Other indications include lowered risks of urinary tract or foreskin infection, sexually transmitted disease and penile cancer. The absolute numbers of these risks are low, for example, the risk of urinary tract infection is 1 out of 1,000 patients for circumcised boys, and 1 out of 100 for uncircumcised boys. There are risks of the procedure which are discussed below.
Should my baby boy have a circumcision?
When boys are born, their foreskin is too tight to be pulled back over the head of their penis. This condition, called physiological phimosis or non-retractile foreskin, typically resolves itself with age, with the majority of boys able to retract their foreskin by the time they are five years old.
The decision for circumcision during infancy is a personal one. The American Academy of Paediatrics Circumcision Policy Statement recognizes the health benefits of circumcision but does not deem the procedure to be a medical necessity for the well-being of the child (1). Many parents from America, Australia and Philippines were circumcised when they were newborn and it is culturally acceptable. The Jewish and Arabic religions also propose it to be performed within 7 days of life.
When is the best time for circumcision?
The best time for circumcision remains controversial, and is strongly influenced by religious and cultural beliefs. It is performed during infancy, as a boy or as an adult. In the newborn or infant, the circumcision can be performed without general anaesthesia (GA), hence avoiding general anaesthetic risks.
Secondly, there is minimal memory of the procedure having been performed. However, there are risks of secondary tightening of the foreskin (phimosis), skin bridges, Plastibell dislodgment, bleeding, urinary opening (meatal) stenosis and need for a repeat procedure. Meatal stenosis or secondary phimosis is due to ammonia dermatitis from the exposure of the penis to the urine sodden diaper.
In childhood, there is the need for general anesthesia when the child is unable to cooperate and stay still. With age comes memory and stress post surgery. Conversely, when the child is able to cooperate, the operation can be performed under local anaesthesia, without need for GA.
Now, my son has grown up and has possible infection of the foreskin. Should he have a circumcision?
Your son should be examined by a paediatrician or a paediatric surgeon. During an acute infection of the foreskin, treatment is oral antibiotics and painkillers. After the infection has settled, I will re-examine your child and advice whether circumcision or topical steroid cream should be used to prevent recurrent infection. The benefits and risks of circumcision are as discussed, and the procedure is the definitive treatment to prevent a recurrence. Topical steroid cream is effective in some patients, which is dependent on patient and caregiver compliance and technique. In uncooperative patients, it is difficult to apply the steroid cream and gently retract the foreskin, hence decreasing the effectiveness of treatment. Varying success is reported from 50 to 90% in the literature (2). It is important to know where and how to use the cream to ensure the highest efficacy. I advise applying for a maximum of 4 weeks, because of the potential side effects of skin thinning, ulceration and infection. Recurrent tightening of the foreskin around the urinary tract opening is concerning for worsening of the condition and scarring (balanitis xerotica obliterans).
How is circumcision performed?
In newborns and babies till 6 months old, circumcision can be performed under local anaesthesia with a sleeve method or Plastibell device. I have moved towards doing the modified sleeve circumcision instead of the Plastibell, because there is less risk of excess skin and a secondary phimosis occurring. The baby is awake and has a pacifier with glucose water for comfort. The foreskin is cleaned under antiseptic conditions. Local anaesthesia is given. A sleeve of foreskin is cut circumferentially around the inner and outer prepuce. Circumcision is completed by trimming the excess skin off, and the edges are stitched together after haemostasis (Figure 1).
Alternatively, an appropriate sized Plastibell is selected and placed over the tip of the penis. A string is tied around the Plastibell to constrict the blood supply to the excess foreskin.
In an older boy, I perform a modified sleeve circumcision under local anaesthesia with sedation, or general anaesthesia. The excess foreskin is trimmed and haemostasis is achieved using diathermy (a heat device that seals the blood vessels). The skin is closed with absorbable sutures.
Another instrument used to trim the foreskin is laser, which works on a similar principle of heat sealing of the skin and blood vessels. The outcome of diathermy and laser is the same.
How is the recovery post circumcision:
Please bring along boxer shorts or loose underwear for your child to wear after circumcision. The patient can have normal baths. Washing with tap water or sterile solution after each pee helps keep the wound clean. Minimal bleeding or swelling is expected. Granulation tissue appears as small yellowish areas on or around the head of the penis, because the raw skin is exposed and forms a more mature layer.
In babies, it is advisable to check the diaper 1 to 2 hourly. If the diaper are soiled with pee or poop, please change it to keep the wound clean. If the diaper tends to stick to the wound, a thin layer of Vaseline can be applied to the diaper to prevent this.
If a Plastibell was used, after 3 to 14 days, the Plastibell drops off as the excess foreskin shrivels up. The Plastibell may dislodge too early resulting in bleeding.
In an older boy, the discomfort improves after the 1st day. The painkillers may be required during the first 3 days.
The risks of circumcision include excess bleeding, bruising and infection. Infection presents as increasing redness, swelling, pain, or abnormal discharge from the circumcised site. If any of these occur, treatment is readily available and we can be contacted at [email protected], +65 87727527 or +65 63592679.
What are the costs for circumcision?
We take reference from the Ministry of Health, Singapore, Fee Guidelines. These fees are payable by Insurance, Medisave, Child Development Account (CDA) and Baby Bonus Cash Gift, when applicable. The costs are Medisave payable up to $650 for a Day Surgery procedure (3), and fully payable via CDA when there are sufficient funds. The procedure is done in our operating theatre. The total costing for an uncomplicated circumcision, with normal patient anatomy, includes consultation, medications and standard consumables. They are as follows:
The estimated total cost for circumcision in a newborn baby until 3 months old, is $1000, subject to the prevailing Goods and Services Tax (GST) rate. This is performed under local anaesthesia.
The estimated total cost for circumcision in a child between 3 months to 6 months old, is $2200, subject to the prevailing Goods and Services Tax (GST) rate. This is performed under local anaesthesia.
The estimated total cost for a child more than 6 months old, will be updated during the consultation. This is because in an older child, I will perform a history and physical examination to identify indications for circumcision and alternative therapeutic options. When needed, there is an anaesthetist, who will provide sedation or general anaesthesia.
When there are complications for example, allergy (not previously known) to medications used, or abnormalities found during the removal of the foreskin, for example a penile torsion or megameatus intact prepuce, the costs differ. I correct these abnormalities during the same general anaesthesia. However this is not possible when the circumcision is performed under local anaesthesia, and a staged procedure is then required.
References
(1) Circumcision policy statement. American Academy of Pediatrics. Task Force on Circumcision. Pediatrics. 1999 Mar;103(3):686–93.
(2) Moreno G, Corbalán J, Peñaloza B, et al. Topical corticosteroids for treating phimosis in boys. Cochrane Database Syst Rev. 2014 Sep 2;(9):CD008973.
(3) https://www.moh.gov.sg/cost-financing/healthcare-schemes-subsidies/medisave
Share if you like this post
If you have other enquiries on children’s surgical conditions, feel free to contact us

Paediatric Surgery & Urology International
© Copyright- 2023 Childsurgery.sg
All Rights Reserved
